Improving primary care for people with mental illness
Our Aim
The overall aim of this project is to develop standards for virtual delivery of mental health services for mild/moderate anxiety and depression within Canadian primary care. Ensuring equitable, high quality, accessible care for these common conditions is
a key health system objective that can facilitate achieving the Quadruple Aim. These standards will represent a benchmark for what constitutes high quality mental health care in Canadian primary care, with patient perspectives and experiences at their
core.
Project overview
Overall Goal: To develop benchmarks for what constitutes high quality, equitable virtual care in the Canadian primary care context for common mental illnesses (anxiety, depression, severe mental illnesses; excluding addiction)
The framework of this project is built on the Quadruple Aim. The Quadruple Aim can be compared to a compass in that it points the way forward for the health system as a whole, including patients and providers.
Quadruple Aim 1 is Improving patient and caregiver experience; enhancing patient satisfaction and improving continuity of care; supporting care coordination. Quadruple Aim 2 is Improving population health; enhancing prevention and effectively managing common health issues. Quadruple Aim 3 is Reducing healthcare costs; increasing resource utilization efficiency and reducing unwarranted variation and Quadruple Aim 4 is Improving provider experience; reducing provider burden, improving efficiency and workflows, and reducing burnout.
The project is going to be in 3 phases.
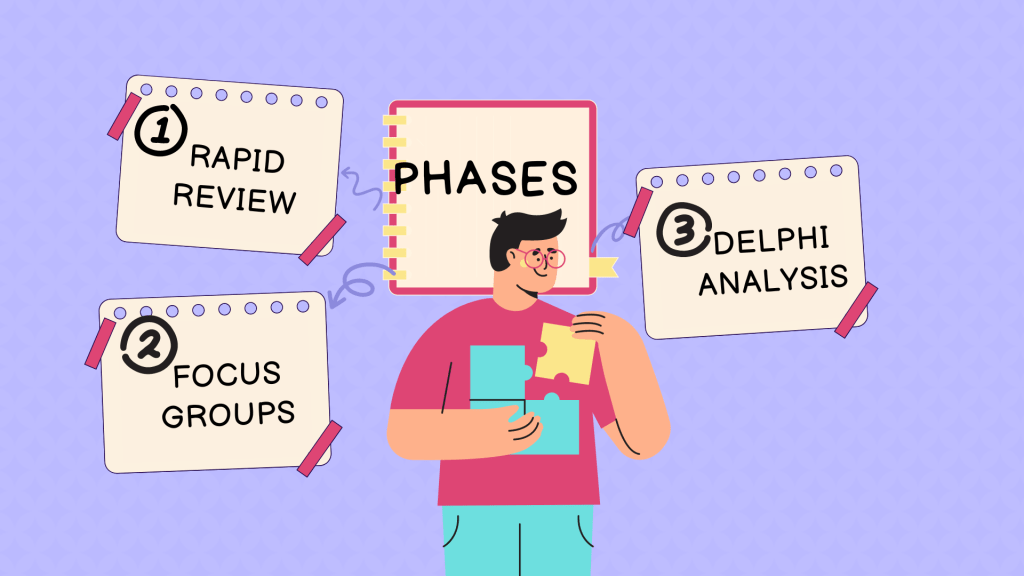
PHASE 1
Rapid review of international resources to identify best practices in countries with similar health systems; generate potential standards for Canadian jurisdictions.
Outputs: Rapid review protocol paper, Rapid review manuscript, List of candidate recommendations and key issues for Phase 2
PHASE 2
Focus groups with stakeholders (family doctors, people with lived experience of mental illness, psychiatrists, other mental health professionals) – explore reflections on rapid review findings and how to apply to Canadian context
PHASE 3
Delphi consensus process with stakeholders (people with lived/living experience and primary care providers) to assess recommendations from Phase 1 feasibility and relevance.
Outputs: List of feasible and acceptable recommendations for virtual delivery of mental health services in Canadian primary care settings.
Questions?
Braden.Oneill@unityhealth.to

